Introduction
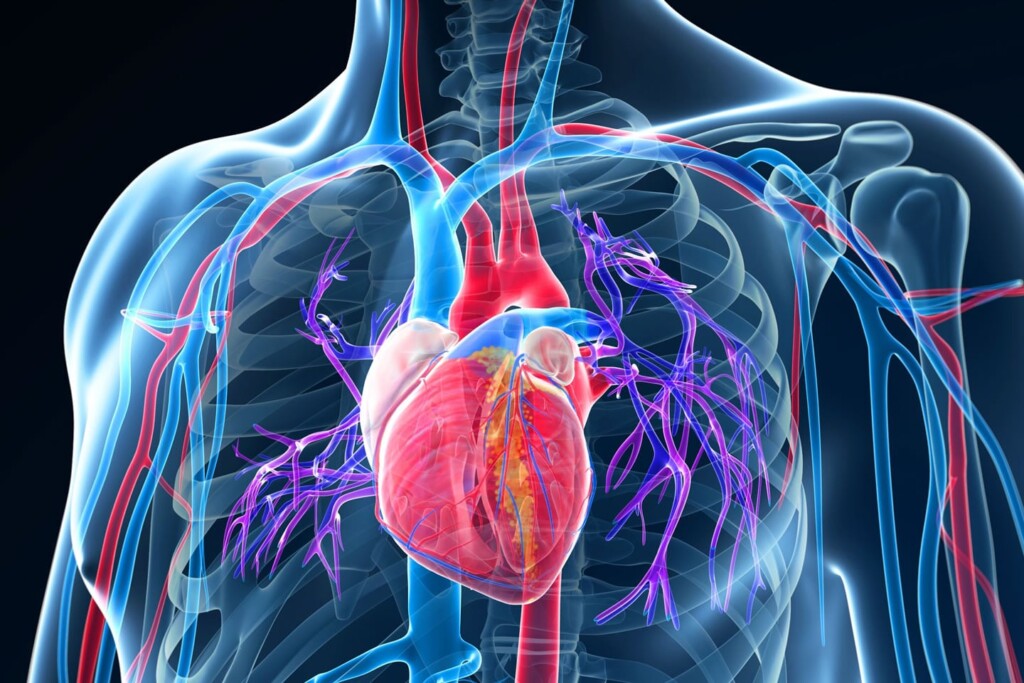
Cardiovascular diseases (CVDs) are the leading cause of death worldwide, responsible for an estimated 17.9 million deaths annually, according to the World Health Organization (WHO). These diseases affect the heart and blood vessels, leading to conditions such as coronary artery disease, heart failure, stroke, and hypertension. Understanding the signs, symptoms, prevention, and treatment options is crucial for managing and reducing the risk of these life-threatening conditions.
Overview of Cardiovascular Diseases
CVDs encompass a range of conditions affecting the heart and circulatory system, including:
- Coronary Artery Disease (CAD): Narrowing of the arteries due to plaque buildup, increasing the risk of heart attack.
- Hypertension (High Blood Pressure): Persistent elevation of blood pressure, leading to heart failure, stroke, and kidney disease.
- Heart Failure: The heart’s inability to pump blood efficiently, causing fatigue and shortness of breath.
- Stroke: A blockage or rupture in a blood vessel supplying the brain, leading to neurological damage.
- Arrhythmias: Irregular heartbeats that may cause dizziness, fainting, or even sudden cardiac arrest.
Statistics on Cardiovascular Diseases
- Global Impact: CVDs account for 31% of all global deaths, making them the most significant cause of mortality worldwide (WHO, 2023).
- United States: The Centers for Disease Control and Prevention (CDC) reports that nearly 697,000 people in the U.S. died from heart disease in 2022—about 1 in every 5 deaths.
- Economic Burden: The estimated global cost of CVDs exceeds $1 trillion annually, with healthcare expenses and lost productivity contributing to economic strain (American Heart Association, 2023).
Signs & Symptoms of Cardiovascular Diseases
Early detection of CVDs is crucial in preventing severe complications. Common symptoms include:
- Chest pain or discomfort (angina): A feeling of tightness, pressure, or burning in the chest, often triggered by physical exertion.
- Shortness of breath: Difficulty breathing, especially during activity or while lying down.
- Fatigue: Persistent tiredness or weakness, even with minimal effort.
- Dizziness or fainting: Sudden episodes of lightheadedness or unconsciousness due to poor blood circulation.
- Irregular heartbeat (arrhythmia): A fluttering or rapid heartbeat that may indicate an underlying cardiac condition.
Causes and Risk Factors
Several factors contribute to the development of CVDs, including:
- Lifestyle Factors: Poor diet, lack of exercise, smoking, and excessive alcohol consumption.
- Medical Conditions: Hypertension, diabetes, obesity, and high cholesterol increase the risk of heart disease.
- Genetics: A family history of heart disease can predispose individuals to cardiovascular issues.
- Aging: The risk of CVDs increases with age, particularly after 50 years.
Treatment and Cure
While some CVDs can be managed effectively, others require medical intervention. Treatment options include:
1. Medications
- Statins: Reduce cholesterol levels to prevent artery blockages.
- Beta-blockers: Lower heart rate and blood pressure to ease the workload on the heart.
- ACE Inhibitors: Help relax blood vessels and reduce blood pressure.
- Blood Thinners (Aspirin, Warfarin): Prevent blood clots and reduce stroke risk.
2. Medical Procedures and Surgeries
- Angioplasty and Stenting: Opens narrowed arteries using a balloon and places a stent to keep them open.
- Bypass Surgery: Redirects blood flow around blocked arteries.
- Pacemaker Implantation: Regulates irregular heartbeats.
- Heart Transplant: A last-resort option for severe heart failure cases.
3. Lifestyle Modifications
- Dietary Changes: Adopting a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins.
- Regular Exercise: At least 150 minutes of moderate exercise weekly can improve heart health.
- Stress Management: Practices such as meditation, yoga, and deep breathing can help reduce stress.
- Quitting Smoking & Limiting Alcohol: Smoking damages blood vessels, while excessive alcohol raises blood pressure.
Prevention of Cardiovascular Diseases
Prevention is the best strategy to combat CVDs. Key measures include:
- Maintaining a Balanced Diet: Reduce intake of saturated fats, trans fats, and cholesterol.
- Engaging in Regular Physical Activity: Exercise strengthens the heart and improves circulation.
- Avoiding Tobacco and Excessive Alcohol: Both contribute to high blood pressure and heart damage.
- Managing Stress Effectively: Chronic stress increases the risk of hypertension and heart disease.
- Monitoring Blood Pressure and Cholesterol Levels: Regular check-ups help detect risk factors early.
Research and Advances in Cardiovascular Health
Medical advancements are continuously improving CVD diagnosis and treatment. Some recent breakthroughs include:
- Gene Therapy: Scientists are exploring gene-editing techniques to repair heart tissue damaged by heart attacks (Harvard Medical School, 2023).
- AI and Wearable Technology: Smartwatches and AI-driven diagnostic tools can detect early signs of heart disease (Journal of the American College of Cardiology, 2023).
- Stem Cell Therapy: Ongoing research suggests that stem cells may help regenerate damaged heart tissue (Mayo Clinic, 2023).
Conclusion
Cardiovascular diseases remain a significant global health concern, but with proper preventive measures, lifestyle changes, and medical interventions, the risk can be significantly reduced. Early detection and proactive management play a crucial role in maintaining heart health. By prioritizing a healthy lifestyle and staying informed on the latest medical advancements, individuals can take charge of their heart health and lead longer, healthier lives.
References
- World Health Organization. (2023). Global Health Reports.
- Centers for Disease Control and Prevention. (2023). National Health Statistics Reports.
- American Heart Association. (2023). Cardiovascular Disease Statistics.
- Harvard Medical School. (2023). Advances in Cardiac Gene Therapy.
- Mayo Clinic. (2023). Innovations in Heart Failure Treatment.
- Journal of the American College of Cardiology. (2023). AI in Cardiovascular Medicine.